In the United States alone, approximately 5-20% of the population contracts the flu every year, with over 200,000 people hospitalized due to its complications, and around 36,000 deaths. The main cause of death is not the flu itself but the complications that follow. Higher risk groups for contracting the flu and developing complications include primarily children under 2 years old, the elderly, as well as individuals with weakened immune systems, chronic diseases—especially of the respiratory and circulatory systems—and diabetics.
Influenza virus exists in three types: A, B, and C. The most dangerous is type A, responsible for outbreaks of epidemics that recur with varying severity, usually every 1-3 years. This type can cause the flu not only in humans but also in animals (horses, seals, whales, pigs, poultry). A characteristic feature of type A influenza virus is its remarkable ability to change its structure (antigenic shift), which makes fighting it a constant challenge. The virus can rapidly alter the protein structure of its envelope, meaning that antibodies from previous infections may not recognize new strains. Consequently, a person can get the flu multiple times in their life.
Type B virus only infects humans, causing milder flu but can still trigger epidemics. Type C infects humans and pigs, does not cause epidemics, and results in the mildest form of flu.
Influenza viruses spread via droplets—transmitted through contact with respiratory secretions of infected individuals during talking, coughing, or sneezing. They can also spread through facial contact, hands, and surfaces contaminated with infected saliva droplets. According to existing data, one sick person typically infects about 1.4 to 1.8 others. This rate is significantly higher in enclosed spaces such as offices, cinemas, subways, and shopping malls.
The primary entry points for the viruses into the body of a healthy person are the upper respiratory tract (nose, mouth), where they invade epithelial cells. There, they multiply, and within about 6 hours, new viral particles are released, capable of infecting other cells. Infection leads to the death of these cells. In many patients, the damage to the respiratory epithelium is almost complete, which facilitates secondary bacterial infections. The epithelium regenerates very slowly, sometimes taking up to a month after recovery, which can result in persistent, chronic cough.
Influenza viruses can also spread through the bloodstream and lymphatic system to lymph nodes, the liver, spleen, heart, kidneys, and nervous system. Therefore, complications after the flu can be severe.
Symptoms of the flu include high fever up to 39-41°C, headache, sore throat, muscle and joint pains (characteristic “bone-breaking” pain), sore throat, cough—initially dry, later producing large amounts of sputum—stuffy nose, and significant weakness that can last up to two weeks after recovery.
Children are also more likely to experience gastrointestinal symptoms such as nausea, vomiting, diarrhea, and fever escalation can trigger febrile seizures and hallucinations.
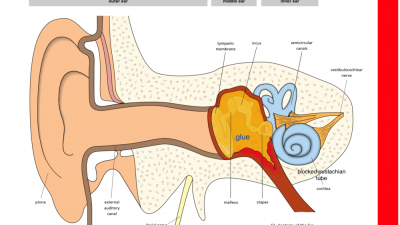
Post-flu complications include bacterial pneumonia, ear infections, sinusitis, worsening of bronchial asthma, myocarditis, circulatory and respiratory failure, sudden death, brain and meningitis inflammation.
Fortunately, not every cold is the flu. The common cold features a gradual onset of symptoms and a runny nose, which is not typical for the flu and does not occur in every case. The illness is generally milder, and complications are rare. To distinguish these illnesses and confirm flu infection, specific tests are available, which are simple to perform by taking a nasal swab.
Uncomplicated flu only requires symptomatic treatment: bed rest, plenty of rest, drinking large amounts of fluids, fever reducers, and cough syrups. Home remedies and herbal medicines can also be used.
Note: Children under 12 years old should not take aspirin or its derivatives due to the risk of Reye’s syndrome, a potentially fatal condition.
Managing flu in daily life involves maintaining so-called broad hygiene practices, which go beyond basic hygiene. This includes rational nutrition, plenty of natural vitamins from vegetables and fruits, daily outdoor activity, adequate sleep, and strengthening the immune system.
There is also a flu vaccine. Vaccinated individuals develop immunity within 7 days and are protected for a year. Antiviral medications are mainly used for high-risk groups.
To prevent getting the flu:
-
Get vaccinated, especially if you belong to high-risk groups or are prone to flu complications (children under 2, the elderly, pregnant women or planning pregnancy, people with weakened immune systems, or with chronic diseases—mainly respiratory and circulatory, diabetics). The vaccine is updated annually to match the anticipated strains of the virus.
-
Take care of yourself: strengthen your body, eat sensibly, stay active outdoors daily, and get enough sleep.
-
Avoid crowded places (theaters, cinemas, museums, shopping centers, stadiums, subways).
-
Wash your hands frequently—up to 10 times a day. Always after using the toilet, returning home, before eating, and after blowing your nose. Wash thoroughly with soap and water for about 20 seconds. You can also use alcohol-based disinfectants, rubbing until hands are dry.
-
Cover your mouth with a tissue when coughing or sneezing to protect others.
-
If you're feeling sick, stay home. Use "home remedies," i.e., bed rest, plenty of fluids, fever reducers, and cough syrups.
-
If symptoms worsen, see a doctor. Follow the doctor’s instructions and take prescribed medications properly. Remember, antiviral drugs are most effective in the first days of infection.
All content on this website is the intellectual property of Poland Medical Clinic. Copying, reproduction, or dissemination in whole or in part, in any form or manner without the administrator’s permission, is prohibited; any unauthorized use will be considered a violation of copyright laws.